A Pandemic Landscape of Optimism and Uncertainty
Throughout the pandemic, we have been checking in with Dr. Howard Forman, a public authority on COVID-19 and healthcare policy, to get his take on the fight against the virus. Nationally, infection rates are close to their low point and many Americans are resuming their usual activities, but the more transmissible Delta variant is spreading and vaccinations are still low in some areas. We asked Dr. Forman where things stand now.
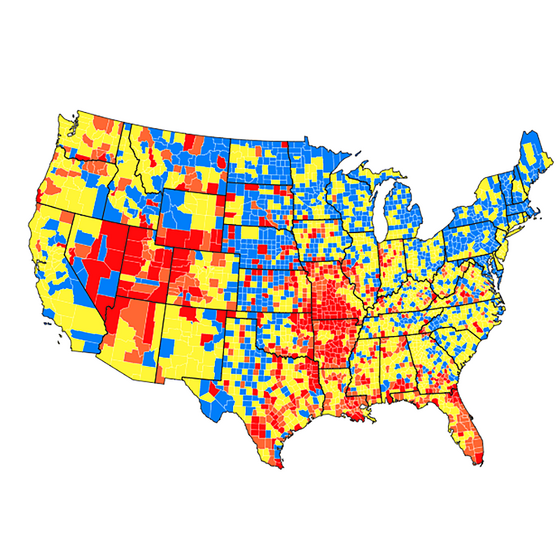
A Centers for Disease Control graphic showing the level of community transmission of COVID-19 from June 29 through July 5, 2021.
We’re realizing that, as Dr. Anthony Fauci says, we’re starting to live in two Americas, one with high vaccination rates, one with low. Is COVID turning into a regional disease?
“The current small waves sweeping through many states seem to be almost exclusively occurring in regions that are under-vaccinated and sparing those that have much higher vaccination rates.”
Throughout the pandemic, COVID has been regional but sweeping. First in China and Korea, then in Europe and hotspots in the United States (New York, New Jersey, Connecticut, Massachusetts, Rhode Island the worst among them), and then almost every state in the country at one time or another. The vaccine has changed some of the narrative: it is now not enough to talk about states, but we must look at counties and cities. The current small waves sweeping through many states (including Missouri, Nevada, Utah, and even California) seem to be almost exclusively occurring in regions (typically rural) that are under-vaccinated and sparing those that have much higher vaccination rates.
Can people in those high-vaccination areas go back to “normal”? Or should they still be taking precautions?
The risks to a vaccinated individual, at present, are very low: they have a lower likelihood of infection, and substantially lower risks of severe disease, hospitalization, death, and even long COVID (as best we can tell). But this is still far from normal: they will interact with friends, family, coworkers, customers who may choose to be unvaccinated or have lower immunity to begin with, or may be ineligible for vaccination. For indoor activities that involve unvaccinated individuals (or unknown status) and close proximity, wearing a mask will help reduce spread if you are infected but asymptomatic. We should also continue to make progress on appropriately ventilating indoor spaces so that the fall and winter are safer for all. We must come to some level of comfort with a new normal.
What do we still not know?
We still don’t know whether the Delta variant is more virulent (that is, more harmful to the individual), but we do believe that current vaccines remain effective against it. We have not seen the last of the variants: will one be more infectious and substantially less virulent? Will one evade existing vaccines? Will we require booster shots? Do previously infected individuals require one shot, two shots, no shots? We must remain humble: we will not have definitive answers to some of these questions, or might get them too late to be of real use. We rely on existing science, inference, and continued data collection, analysis, and policy recommendations from our best and brightest scientists. The list of known unknowns is vast; the “list” of unknown unknowns may be infinite.