Sandeep Jauhar: A Witness to Dementia
Subscribe to Health & Veritas on Apple Podcasts, Spotify, YouTube, or your favorite podcast player.
Howie and Harlan are joined by Sandeep Jauhar, a cardiologist and the author, most recently, of the memoir My Father’s Brain: Life in the Shadow of Alzheimer’s. Harlan reports on new research about the timing of blood thinners for stroke patients with atrial fibrillation; Howie checks in on two physician groups that were acquired by private equity investors earlier this year and are now facing bankruptcy.
Links:
“Early versus Later Anticoagulation for Stroke with Atrial Fibrillation”
Sandeep Jauhar: Heart: a History
Sandeep Jauhar: “How Would You Feel About a 100-Year-Old Doctor?”
Sandeep Jauhar: My Father’s Brain: Life in the Shadow of Alzheimer’s
“The Dutch Village Where Everyone Has Dementia”
National Institute on Aging: What Causes Alzheimer's Disease?
“KKR-Backed GenesisCare Preps for Bankruptcy Filing Within Days”
“KKR-Backed Envision Healthcare Plans Chapter 11 Bankruptcy Filing”
Learn more about the MBA for Executives program at Yale SOM.
Transcript
Harlan Krumholz: Welcome to Health & Veritas. I’m Harlan Krumholz.
Howard Forman: And I’m Howie Forman. We’re physicians and professors at Yale University. We’re trying to get closer to the truth about health and healthcare. This week we’ll be speaking with Dr. Sandeep Jauhar, but first we like to check in on current topics in health and healthcare. So what’s got your attention this week, Harlan?
Harlan Krumholz: Yeah, thanks, Howie. And we’re looking forward to this interview with Sandeep, but I want to jump into a paper that was published in The New England Journal of Medicine first. And it’s just an example for people listening of how many things we don’t know that are really important details in the care of patients. So if I ask you, somebody comes in with a stroke and they’re diagnosed with atrial fibrillation during the stroke. So we believe that, as you know, that irregular heart rate can lead the upper chamber of the heart to develop blood clots, which can be pushed out and end up in the brain and cause a stroke. And so that’s why a lot of people get their blood thinned, anticoagulants, when they have atrial fibrillation to prevent these strokes. Now here’s, somebody comes in, nobody knew they had atrial fibrillation, they have a stroke and they’re diagnosed with atrial fibrillation.
Question is, when should you start the blood thinner? When would be good to get them on a blood thinner? And the reason it’s a question at all is because there’s been some concern that when you have a stroke that if you give a blood thinner, if you give this anticoagulant to people, you can have what’s called a hemorrhagic conversion. That is, you take a stroke, that was because their blood clot formed and it deprived a part of the brain of blood, with the blood thinner, that damaged tissue could start to bleed and then they can start to actually get an intercranial hemorrhage. It’s inside the brain, you can get a bleed, which could be catastrophic. So people have often thought you need to wait a couple days. And actually they did a trial here where they took people that came in and they randomized them to more rapid anticoagulation.
So if you had a minor or moderate stroke, they began the anticoagulation within 48 hours, within the two days. And if you had a major stroke, they started it on day six or seven a week later. Now, that’s in contrast to the normal situation. Or if you have a minor stroke, people are usually waiting three or four days, a moderate stroke, six or seven days, and a major stroke, they might wait two weeks. Now that may just seem like a couple days, but it’s an important decision where you’re taking care of patients because you want to protect them against more blood clots going to the brain. On the other hand, you don’t want to get this bleeding in the brain. And guess what, when they did this study, very interesting, they enrolled about two thousand people, had a lot of different sites all across the world.
And what they found out was that the earlier treatment actually seemed to produce a better outcome. Now, the way they did this trial, they provided a range of benefits. So the benefit was as much as almost three-percentage-point benefit from an outcome that they were looking at, for example, recurrent stroke. But they also included issues of bleeding. So they added all this together, systemic embolism, which means a blood clot went somewhere else or vascular death within thirty days after randomization. And so the more rapid treatment on average was better, could have been as much better as a benefit for every thirty-three people treated maybe at the bottom side for every two hundred people treated, but largely not a big downside. And the hemorrhagic part, the bleeding part that people were worried about was pretty rare in both groups. So anyway, I’m just bringing this up because it’s just, we need to be doing tons of these kinds of studies. I mean, all this time later, we’re not sure when to start the blood thinner on people coming with a stroke in atrial fibrillation. Studies like this all of a sudden start filling in the cracks of our ignorance and are so important to start being able to ask these very simple questions. But they are critically important to so many patients around the world.
Howard Forman: Yeah. Now it’s grateful to see people investigating these things. There’s so many questions. I periodically have A-fib. I’ve had family members ask questions about this, and it’s amazing to me how much indecision there is about a lot of features about treating A-fib when you start and stop anticoagulation and so on.
Harlan Krumholz: Yeah. Yep. So anyway, just wanted to share with folks because it was just one of these things that has baffled the profession, and now there’s some good evidence. But hey, let’s get onto the interview with Sandeep.
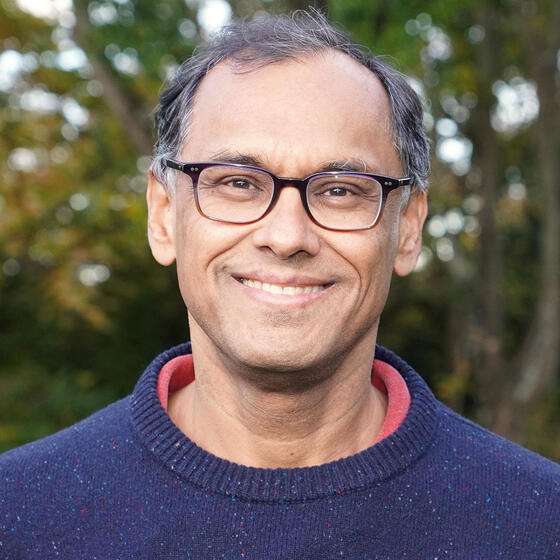
Howard Forman: Dr. Sandeep Jauhar is a practicing heart failure cardiologist at North Shore LIJ Hospital. Most recently, Dr. Jauhar has written My Father’s Brain: Understanding Life in the Shadow of Alzheimer’s, a memoir about his experience with his father’s dementia. This is his fourth bestseller. He is a contributing opinion writer for The New York Times, focusing on medicine, health, aging, and ethics. He has also appeared frequently on National Public Radio, CNN, and MSNBC and contributed to various publications such as The Wall Street Journal, The Washington Post, and The New England Journal of Medicine. Dr. Jauhar holds a bachelor’s and a PhD in physics from the University of California Berkeley and an MD from Washington University School of Medicine in St. Louis. He completed his residency at New York Hospital, Weill Cornell Medical Center, and a cardiology fellowship with a specialization in heart failure at New York University School of Medicine. So first, welcome to the Health & Veritas podcast. I usually go right into the first question, but in this case, I need to duly note that Harlan brought you and your book to my attention, And I know he wanted to relate why this was so important to him and should be to our listeners. So I’m going to let Harlan take it away from here.
Harlan Krumholz: I said to Howie, Sandeep, that this was important to me personally because of what I went through with my father who was a physician and really a large influence on my life course—that understates it, I choked up kind of thinking about this—but who was beginning to this sort of giant of a man in my world experienced this cognitive decline and in contrast to your father. And his parents also had experienced some of this, I think through COVID, he got ill and he just stopped eating. But anyway, I want to thank you for writing the book. It meant a lot to me to read it. I’m sure others will have the same experience. And I just wonder if you could just tell us a little bit about, you experienced this, what brought you to actually spend the time and devote yourself to reliving it and writing about it and then sharing it?
Sandeep Jauhar: Yeah, I mean, I got an email after my publisher sent an advance copy to one of the real titans in the field of dementia, and he wrote back and said, “Most people, after going through what you’ve been through, don’t even want to think about it anymore. But you’ve provided a very important public service in wanting to write about it.” And actually, I never really wanted to write about it. My father got sick in 2014. Well, that’s when he was diagnosed by a neurologist. He had been living in Fargo, North Dakota, working as a research scientist, running a lab, having postdocs and graduate students running a greenhouse, doing microscope work. I mean, really, by all indications, he was doing fine. I was living in New York, and so was my brother. We went through a very long journey with him for seven years before he died.
And I would say that really, it was only toward the end, so probably sort of around the time of COVID actually, that I thought about writing this book. I had been doing a lot of research about Alzheimer’s and dementia, mainly to try to understand what was going on with my dad. He was a brilliant man who became severely cognitively as well as emotionally impaired. And it was very difficult for me to process. There were times when I was very impatient, and for me, at least as a scientist, as a doctor, I needed to know what was going on with him on a neurological level to help inform my caregiving. And so many years later, when he was really declining, I thought, “This has been the most difficult journey I’ve ever taken.” So I ended up writing the book that I needed, that I didn’t have through this journey, A book that’s both about the personal aspects but also provides sort of a neurological script for what goes on in dementia and Alzheimer’s with the intent of...that knowledge is power but also knowledge provides comfort and patience. And I think patience is in real short shrift when you’re a caregiver for someone with Alzheimer’s.
Howard Forman: And let me just say for our listeners that the book is a layered approach to writing that I don’t think I’ve ever seen done so well. I mean, you cover the basic science that we know about with Alzheimer’s and cognitive function even before Alzheimer’s. You then use very personal and poignant narratives about your own experiences. You have clinical narratives from doctor’s offices. And I’m just wondering how were you able to keep track of all that over the years? You have this from 2014 up until I think early 2021. Were you journaling during this time? Did you anticipate that you would be writing this?
Sandeep Jauhar: I did not anticipate I’d be writing this book. I was working on a different book for a large portion of this time. It was a book called Heart: A History, which came out in 2018, the fall of 2018.
Howard Forman: Also a bestseller.
Sandeep Jauhar: Yeah. And I’d say around the time that Heart came out, I started doing a little bit of journaling. For me, journaling is just a way of recording my experience. It doesn’t necessarily mean I’m going to write about what I’m journaling about, but I’ve been a fairly prodigious journaler for most of my writing career. I mean, I started when I was in graduate school, and I like to journal because it helps me clarify my thinking about things. And with my father’s disease, there was just so much that was mysterious to me that needed clarification. I write in the book that, I mean, when my dad was diagnosed by a neurologist with MCI, which is mild cognitive impairment, honestly—and I’m embarrassed to admit this, I mean, I went to medical school after all—I didn’t even know what MCI was. I had never even heard the term. I mean it’s a sort of pre-dementia.
But when he said, this is mild cognitive impairment, the first thing I did when I got home is read up on it. What does it mean? What are the chances that this is going to progress? What are the chances that this is in fact what we suspected at that time, that it’s Alzheimer’s? So I just found myself sort of butting against my ignorance over and over with regard to the brain and dementia and memory. Why was my father becoming so emotionally labile? Why did he have a lack of self-awareness toward the end? What was going on in the brain that served, underlay, that clinical syndrome? All those things spurred me to do a lot of reading and a lot of journaling. But I’d say that I didn’t really know I was going to write this book until probably sometime during the COVID period.
Harlan Krumholz: I want to explore a couple different themes with you. One of them is this issue about the diagnosis of mild cognitive impairment. Once you have that diagnosis, then all of a sudden the person with that diagnosis gets marginalized, and as much by their disease as our response to them. And so it’s no wonder that people aren’t eager to have someone start to label them with cognitive dysfunction. And I find it in tension, because on one hand we want people to be diagnosed so that we can respond appropriately, plan, help, support, assist, facilitate. On the other hand, once you get that label, everyone’s interactions with you I think do change. I mean, I noticed it in our family.
Sandeep Jauhar: Yeah. So it was very clear. I mean it actually was very clear to my mother. She was the one who actually told us to take my father to a neurologist because we had gone on a walk and she said, “Your dad got lost driving to Sears the other day. And instead of calling one of you, his sons, he stopped the car on the road and actually wandered out into incoming traffic to try to stop a car to ask for the way home.” So the neurologist said, “Given the history you’ve given me, given the history your dad was unable to provide, and then given the scores on the Mini-Mental Status Exam as well as other neurological testing, it’s pretty clear that he has mild cognitive impairment.” Now the larger issue is, what do you do with that diagnosis and how do you respond to it as a family?
And I would say that what you mention is something that I wrote about a lot in the book, about there came a point where I just didn’t trust my father to have even a normal thought anymore. And that was horrible, both for me as a caregiver, but I can only imagine how bad it was for him as a brilliant man. But it was just very hard to see him in the same way after he got this diagnosis. And a part of that is what I write about in the book, is sort of our hyper-cognitive culture where what we prize in the western world, really all over the world, is sort of individualism and ability to process information, ability to be economically productive. And when my father lost the ability to do those things, he became marginalized, not just by the outside world, which kind of fled from him once it was clear that he was declining from Alzheimer’s, but even his own family. I mean, we had a really hard time dealing with it.
Howard Forman: I want to pivot from that topic to a related topic. And you wrote a New York Times opinion piece less than six months ago, I think, or around six months ago on how would you feel about a 100-year-old doctor? And I just wanted to bring that up because I’ve sort of faced this with my own family. My mother needed a knee replacement about two years ago, and the person that everybody said was the best was 80 years old. And I was a little concerned at first, and honestly, he turned out to be the best surgeon. She’s had two knee replacements, and his was without question the better one. And every outcome I hear about this man is exceptional, but you wrote about this and what people should anticipate and what our system should anticipate as our medical professionals also age. Do you want to just say a couple of words about your thoughts on that?
Sandeep Jauhar: Yeah, I mean, look, dementia, cognitive impairment are growing and by now massive public health problems. I mean, one out of every 10 Americans over the age of 65 has dementia or a related Alzheimer’s or some related dementia. So there’s no reason to think that doctors are completely immune to that. There is something to be said for having cognitive reserve, something to be said for education. And obviously economics play a role. People who are wealthier tend to be buffeted from the sort of slings and arrows of disease and social responses to disease. But the point is that there may be fantastic surgeons who are 80 years old, and I’ve certainly met my share of very young doctors who I wouldn’t trust to take care of my family. But the reality is that with aging does come cognitive decline, that’s just a truism. And does it happen to everyone at the same rate?
Obviously not. So my argument is that we need to be prepared because doctors are working longer. In the article, I mentioned a 100-year-old neurologist who seems to be a wonderful person. I interacted with him—certainly very, very sharp. But even if he is, he’s really the exception. I think most doctors or most people at the age of 100 are going to have significant cognitive impairment. So the argument is that we should have competency testing like we do for pilots. I mean, well, for pilots actually, we don’t have competency testing. We actually mandate retirement age. And I certainly don’t want to do that for doctors because people age at different rates. But I do think that competency testing is a worthwhile thing to explore. And not just for doctors but for lawyers and accountants and even politicians. Anyone who has people’s lives or livelihoods in their hands, we should make sure that they’re cognitively intact and they can do the jobs that we’ve entrusted them with.
Harlan Krumholz: We actually have that at Yale New Haven. Alan Friedman, who’s our chief medical officer at Yale Haven Hospital, and Tom Balcezak, our chief medical officer of the entire system, have instituted across the system competency testing starting at age 70. And actually, of course there was some resistance going forward, but now it’s well accepted. I want to hit on just a couple, I’m going to ask a quick thing, I’ll give you back Howie, and then I’ve got one thing to end on. You talk about in the book the fact that for some people, lying to people with cognitive dysfunction is a strategy, and then you come out strongly, and you know how much I resonate with this.
You said quote, “In my own career, I’ve seen how even well-meaning paternalism can be damaging. The doctor-patient relationship is founded on trust, and paternalistic interference not only compromises the relationship but also can erode faith in the profession.” And yet it seems like it’s a legitimate approach—when I say “legitimate,” one that’s accepted by some people—and you even referred it when you saw this nursing home in Europe, you were saying that almost seems like The Truman Show to you, the way it was being set up. What are your reflections on it now with a little bit of distance? I mean, I get it, you’re just trying to allay anxiety when people seemingly persistent in believing something. But maybe we can share a couple thoughts about this.
Sandeep Jauhar: My problem with lying to my father was that I felt it was compromising his dignity. And some of that was informed by my experiences as a doctor being trained.
Harlan Krumholz: And can you just give an example? Maybe the listeners don’t really know.
Sandeep Jauhar: Sure.
Harlan Krumholz: We’re saying “lying,” it sounds so much harsher. It’s really about going along with the story that they’re telling, right? Not trying to correct them, essentially.
Sandeep Jauhar: Yeah. Well, I mean, yeah, to some degree, with my father, a major sticking point was that we had a live-in caregiver and he didn’t want to pay her. He didn’t want us to pay her. He wasn’t handling his finances at that point. And when he would find out that she had been paid, he would get verbally angry. But I insisted on telling him, “Look, Dad. She’s working for us. You know that people who work need to be paid.” I thought that leveling with him was a way for me to tell him, “Dad, you’re still a part of my world.” That “you still deserve to know the truth.” But the problem is that he couldn’t process the truth. And there were other times when telling the truth actually caused him deep, deep anguish. When I would tell him that mom died, and then he would forget and he’d ask me the next day and I’d tell him again, “Dad, I told you. Mom died. No matter what we say, she’s not coming back.” And that caused him in tremendous anguish.
So my brother eventually came around to saying, “Oh, mom’s not here right now, she’s on her way, or she’s on the plane.” Or whatever it is. And I would see that really allayed his anxiety in tremendous ways. So I would say that there is a conception of dignity that I came around to, which is validating someone’s reality, even if it’s not the reality that you share, even if it’s not objective reality, whatever that means. So for my dad, thinking that my mother was still alive, it was a way to prevent tremendous anguish and also the revisitation of anguish, because Alzheimer’s patients do forget. And so I don’t believe in lying to patients, and I don’t do that as a matter of course, obviously. But I do think there’s a difference between lying for someone else’s benefit and lying for your own. And in my father’s case, I think I came around to this view, which is, some people call it therapeutic fibbing, therapeutic deception, validation therapy, but just sort of validating through white lies a person’s conception of reality. There is dignity with that, especially if it prevents pain and anguish.
Harlan Krumholz: Such an important insight.
Howard Forman: You talk a lot about your family as a community supporting your father and your mother, and you talk about clinicians helping you, obviously, but you don’t talk about any larger communities out there. Are there groups, are there communities that people can reach out to, to get support when they’re going through this to share these common experiences and learn from them?
Sandeep Jauhar: I mean, there’s several communities that... so the dementia villages I visited in the Netherlands and just outside Amsterdam, there’s a nursing home, but it’s really built as a small town where people with advanced dementia can live in a very more humane way than we provide in the U.S. and in U.S. nursing homes. They can wander. So one of the big balances or tradeoffs in dementia care and really elder care in general is safety versus autonomy. No one wants someone to wander and trip and break their hip. So we tend to lock them into memory units. In this dementia village, they accept the tradeoff, they accept the fact that people would want to wander and they accept the risk of potentially falling. So it’s a little town. The residents who have advanced dementia live in these homes that are sort of curated to appeal to them and the lifestyles that they’re used to.
They have a classical music room, they have concerts, they have a cafe, they have a little fountain, they have a pond. And the guide said, people said, “Oh, you can’t have a pond.” People with dementia, they’ll climb over the fence and fall into the pond. And he said, “People with dementia aren’t stupid.” They’re not going to climb over a fence and jump into a pond. That’s sort of the American way of thinking about it. But the European way is different. And then they have these caretakers who sort of pose as the barista in the cafe or gardeners, and they’re sort of keeping track of what’s going on, and they help people who get lost get back home. So it is sort of like the movie The Truman Show. It’s almost like a film being made.
Harlan Krumholz: I often thought we should build these communities around the year that you likely remember best. So you have a bunch of communities that are looked like the 1950s. You got a bunch of communities look like the 1970s. It sort of helps people contextually.
I want to just ask you one final thing just for getting to the end. So you say, I’m just going to read from the book. You say, “Like my father, I firmly believed in the importance of genetics and heredity and determination of human fate. And as a disciple of this philosophy, I could not help but worry that what was happening to him was going to happen to me, too.” You talk also about how you guys have a similar body habitus, an approach, and actually some aspects of your personality in his prime reflect kind of how you are. I’m just curious, having gone through this experience, has it changed you in terms of how you think about how you live your life and what your future may hold?
Sandeep Jauhar: Yeah, so there are genetic elements, hereditary elements to dementia, typically in early onset, as you probably know, where there’s a very strong genetic basis for that. In my father’s case, the late onset dementia, there are genetic factors. The—
Harlan Krumholz: But you’re answering as you’re now going to your cognitive scientific brain. I’m asking about your heart.
Sandeep Jauhar: I worry. I worry about what’s going to happen in the future. This was a glimpse of a potential future, and it certainly creates a lot of anxiety in me about what the future holds, not just whether I might develop dementia but then the impact it’s going to have on my family, on my children. And then there are also aspects of advanced directives that I realize now how difficult it is, even to follow an advanced directive when the advanced directive is written, when you’re cognitively intact, like my father’s was. And then when he became really so impaired but didn’t really seem him unhappy, he wasn’t saying, “Look, it’s my time. I want to die.” He was actually seemed pretty happy. And I came to realize that cognitive impairment and happiness are not actually mutually exclusive necessarily. They might be for caregivers with a sort of hyper-cognitive prejudice, like I probably had, where I wondered whether my father’s life was really worth living given the massive decline, the precipitous decline from being an eminent scientist to really just being happy with just a spoonful of ice cream. But for him, his perceptions, his ambitions, all these things shrunk in a way that allowed him to continue to function and seem to be happy. So I think it’s a very difficult issue. And yeah, of course I worry about it. I—
Harlan Krumholz: And I don’t want to make it uncomfortable. I just was pushing because obviously I’ve had the same thoughts, and it did leave me a little bit with “Seize the moment, seize the moment.”
Sandeep Jauhar: And I would say professionally there’s been sort of consequences too. I mean, I was like a lot of doctors, cardiologists, I do heart failure, a lot of my patients die. And when they would get to that point, very often I would withdraw because doctors, we want to fix things, and when someone is terminal and entering hospice care, we often withdraw. And I found in my experience that it was really important for me that my father’s doctor still be involved, still communicate with us. That was a real balm in those final days. And so I aspire to that too now much more than I ever did.
Harlan Krumholz: Yeah. That’s good lesson. Well, thank you so much. Can’t thank you enough. It’s wonderful to talk to you.
Sandeep Jauhar: Yeah, it was great being with you. And yeah.
Harlan Krumholz: Thank you very much.
Sandeep Jauhar: I admire everything you’re doing.
Harlan Krumholz: Hey, that was a terrific interview. I’m so glad that we were able to get him on the show. But let’s turn to your part now, Howie. What’s on your mind?
Howard Forman: So back in early January, we talked about how physician groups were selling out to private equity firms, and this was having untoward effects on the delivery of high-quality care. The references we made at that time were the orthopedic surgery groups. We also mentioned radiology, emergency medicine, so on. The concerns we raised were that these firms were mostly focused on costs and profits and didn’t seem to have the proper incentives for quality access or price. So fast-forward to May, just a couple of weeks ago, and we have just witnessed the first of what turned out to be two massive private equity–backed failures. One is Envision, which remains one of the largest physician staffing groups covering emergency medicine, radiology, anesthesiology, hospital medicine, other physician services. They also own the large ambulatory surgery practice covering a large territory. They have been at the center of numerous controversies but had been bought out by Kohlberg Kravis Roberts, or KKR, in 2018.
KKR is one of the most well-known, well-funded private equity firms in the U.S. So GenesisCare is another private equity–backed firm, also with a substantial stake in this case from KKR, that is about to enter bankruptcy. If you believe news reports, this leading oncology care provider has its largest base of operations in Australia, but they also have significant centers in the U.S., UK, and Spain, companies go bankrupt all the time. And because of leverage, meaning a lot of debt and the reality that these firms are often teetering when purchased, private equity–backed companies have a much higher rate of bankruptcy. But it’s worth briefly reminding our listeners that healthcare management is difficult. And by that I mean that despite the many news reports of individuals getting rich off of healthcar—and many do—we have structural problems in our system right now, that mean that if you don’t have a strong base of patients with commercial insurance, you too might be teetering on the brink of insolvency. You and I have talked about how broken our system is multiple times before, but we have mostly focused on how bad it is for the consumer. And it is bad, but it is also broken from many providers, too many hospitals, physician groups, nursing homes, mental health providers, and so on are struggling to break even, and that is not good for anyone.
Harlan Krumholz: Yeah. I’m so glad you brought this up. I think one of the issues is that people are concerned that because of the perversity of our system, there are certain areas in the hospital or in the healthcare system where there are big margins and there’s some where there are negative margins. And if the private equity comes in and tries to suck out all the high margin, then hospitals are left low-margin. Story’s still going to be told. But I think it’s fair enough to say that some of these investments have gone south and that some have involved risk, and we’ll have to keep our eye on this.
You’ve been listening to Health & Veritas with Harlan Krumholz and Howie Forman.
Howard Forman: So how did we do? Give us your feedback, or to keep the conversation going, you can find us on Twitter.
Harlan Krumholz: I’m @hmkyale, that’s hmkyale.
Howard Forman: And I’m @thehowie. That’s @T-H-E-H-O-W-I-E. You can also email us at health.veritas@yale.edu. Aside from Twitter and our podcast, I’m fortunate to be the faculty director of the healthcare track and founder of the MBA for Executives program at the Yale School of Management. Feel free to reach out via email for more information or on our innovative programs or you can check out our website at som.yale.edu/emba.
Harlan Krumholz: Health & Veritas is produced with the Yale School of Management and the Yale School of Public Health. Thanks to our researchers, Inez Gilles and Sophia Stumpf, and to our producer, Miranda Shafer, they are absolutely amazing. Talk to you soon, Howie.
Howard Forman: Thanks very much, Harlan, and talk to you soon.