A Decision Analysis Approach Points to Better Diagnosis of Prostate Cancer
Prostate cancer is one of the biggest killers of men in the U.S., and early screening by blood test can identify potentially life-threatening disease—but the current biopsy procedures that follow positive blood tests can also lead to frequent overtreatment. A new study led by Yale SOM’s Arthur J. Swersey, using decision analysis techniques, finds that increasing the number of biopsy needles and using probability modeling to analyze the results can help prevent unnecessary treatment while identifying dangerous cancers.
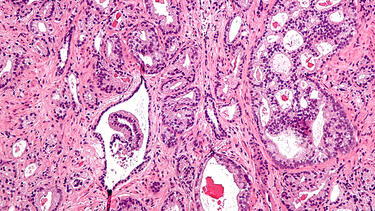
A micrograph showing prostatic acinar adenocarcinoma, the most common form of prostate cancer. Photo: Nephron/Wikimedia.
By Áine Doris
Prostate cancer is the second-leading cause of cancer deaths for men in the U.S. Every year more than 30,000 American men die from the disease. But screening for prostate cancer, a blood test that if positive is followed by a biopsy, is controversial. Proponents argue that screening is the most effective means of catching the disease at an early stage and improving life expectancy for patients. But post-operative analyses show that as many as 40% of patients are being overtreated.
These patients are receiving painful and invasive treatment—surgery and radiation—even though their cancer is not at a stage where intervention is warranted. For these patients, the tradeoffs are serious. Premature cancer treatment is ineffective in treating disease, but the potential side effects—incontinence and erectile dysfunction among them—can be life-changing.
For medical professionals, this represents a genuine dilemma. While overtreatment of insignificant tumors can reduce quality of life, delayed treatment of significant cancers increases the incidence of metastatic disease and death.
New research by Yale SOM’s Arthur J. Swersey may help caregivers and patients resolve the dilemma, using operations research tools—techniques conventionally used to understand and improve industrial and business processes.
With colleagues from Yale School of Medicine, the Cleveland Clinic, Prognos, the University of Iowa, and Indiana University, Swersey created a simulation of the biopsy process and used probably modeling to help make the decision of whether to proceed with treatment or continue with blood-test monitoring. They find that a correctly performed biopsy, combined with proper analysis, could substantially improve the chances of accurately distinguishing insignificant from significant cancers.
Read the study: “Decision models for distinguishing between clinically insignificant and significant tumors in prostate cancer biopsies: an application of Bayes’ Theorem to reduce costs and improve outcomes”
The key, says Swersey, is to use more needles.
In a prostate biopsy, typically, 10 to 12 needles are used to extract tissue from the prostate, which can then be examined by the pathologist to determine the grade of cancer.
Working on the hypothesis that 12 needles may not provide a large enough sample for accurate biopsy, Swersey and his colleagues ran a prostate biopsy simulation, increasing the number and length of needles used.
“Our results are consistent with the principle used in statistics that larger samples provide more information leading to better decisions,” Swersey says.
Using an Excel computer simulation with the prostate represented as an ellipsoid and tumors as spheres, which were randomly located in the posterior part of the gland, Swersey and colleagues simulated the placement of 6, 14, and 20 needles into the prostate.
They then ran a probability model using this data to find a “cut-off point,” the total length of cancer found in the needle cores below which patients should be actively monitored by blood test, and above which treatment by surgery and radiography would be indicated. The decision is always to treat if the pathology of the biopsy tissue is poor, indicating aggressive disease.
“What we found is that 20 needles or thereabouts is the optimal number that should be used to provide a higher volume of tissue in the biopsy,” says Swersey. “Beyond that number leads to diminishing returns, partly because you would need to put your patient under anesthesia. But our key finding is that you do need to use at least 20 needles or so, depending on the size of the prostate, if you want to extract a better, more reliable sample that leads to better decisions. In addition, we found that longer needles also improved the ability to distinguish insignificant cancers from significant tumors.”
So why is the current practice to use only 10 to 12 needles?
Most prostate cancer clinicians believe that inserting more needles into the prostate results in detecting more cancer, including insignificant cancer, without being able to determine whether that cancer is significant and needs to be treated, explains Swersey. So they have been reluctant to increase the number for fear of skewing results even further in favor of intervention.
But Swersey says that the additional data from the biopsy is helpful if it is correctly interpreted, as the probability model does.
“What’s new in our approach is that we run the biopsy data through Bayes’ Theorem,”—a formula to determine the probability of an event based on evidence. That evidence, in this case, is the length of cancer found in the biopsy needle cores. “We consistently found that using larger samples—more needles—as input to our probability model, we got better predictions of whether the cancer is insignificant or not.”
Swersey and his colleagues quantify the costs and benefits of the biopsy while using a different number of biopsy needles, contrasting the negative impact or “cost” to the patient of treating insignificant tumors unnecessarily with the gains in detecting significant cancers. They find that using 20 needles dramatically lowers the costs and increases the benefits.
Swersey acknowledges that the model he and his colleagues have produced is still “simple” and that more research using 3-D simulations that better mirror real anatomy will be needed to hone results further. It does, nonetheless, provide a significant “first step” in using a data-driven approach to making prostate cancer treatment decisions.
“Ours is a simplified model but the insights are enormously valuable. Using this new approach of more and longer needles, and probability modeling to inform decision analysis, we have paved a way for the academic community through more research to follow suit. And taken a significant step forward, I hope, towards improving patient outcomes and ultimately, helping to save lives.”